Lab Protocols: Going Forward in Covid Times
The health and safety of lab workers is at the forefront of all lab design. The COVID-19 pandemic has added enhanced protocols to everything we do, including the way we will work and interact in the lab. The traditional lab worker will need to navigate a multitude of COVID-19 recommendations and safety measures from the time they leave their home to entering the lab. So how do we make the laboratory worker feel safe in this new work environment and provide an enhanced sense of personnel health and safety in the future? Consulting with authorities such as the Centers for Disease Control, World Health Organization, OSHA and an Environmental Health and Safety Officer are primary resources to providing a safe work environment. Current laboratory planning guidelines and standard operating procedures have been documented in literature. However, the pandemic will challenge us to shift paradigms and develop new space planning metrics and SOPs to enhance worker safety.
Lab design:
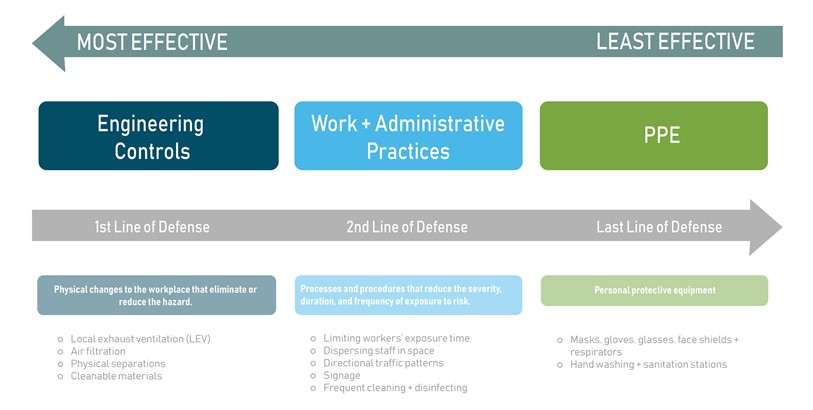
Labs are inherently designed to protect staff from chemical, physical, and biological hazards by using the OSHA’s hierarchy of controls that state that engineering and work practices must be the primary means to reduce risk. Risk = hazard X exposure. Reducing exposure to the hazard, minimizes risk. The following controls help mitigate risk in the lab:
Current engineering controls:
- Demand Ventilation: 100 percent filtered outside air, nothing recirculated
- Provide a negative pressure differential between the labs and public places
- Humidity control 40 to 60 percent may be ideal
- Exhaust devices based on the type of hazard needing to be removed
Added Controls:
- UVGI (Ultra-Violet Germicidal Irradiation) installed at the air handler
- PCO (photocatalytic oxidation, or PCO) reduces airborne virus, biologic and VOCs with every volumetric air change through the system and can be installed in most air handler systems
- Touchless faucets and doors
- Larger space for don and doffing PPE, allowing for social distancing
- Hand washing sinks located by the lab doors. If sinks cannot be added, then provide hand sanitization stations
Current Work Practices:
- Hand washing
- Use of PPE
Added work practices:
- Prioritize hand washing
- Prioritize the use of PPE
- Stage work force
- Regulate days and hours of operation
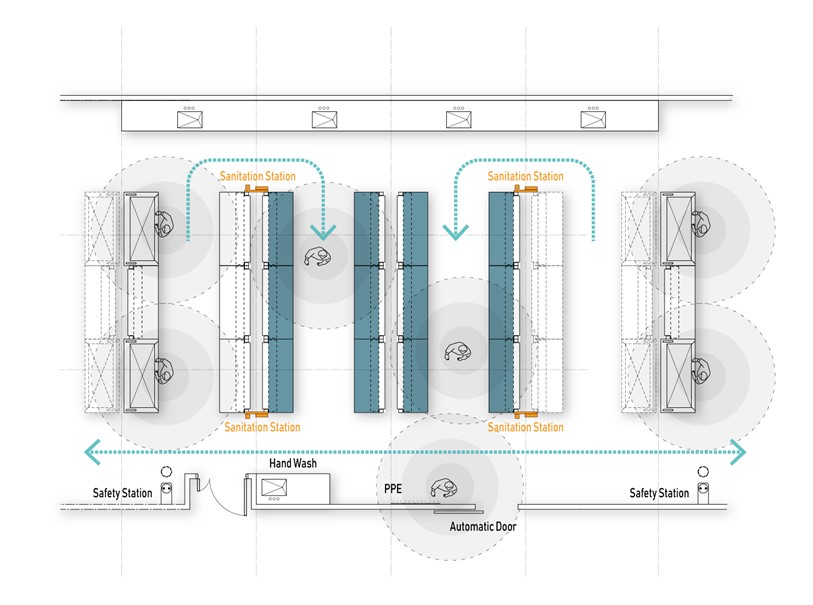
- Develop directional workflow
- Develop cleaning and sanitization protocols
The following is a collaborative effort within the Hanbury organization to identify concepts that could be implemented to provide direction in this time of change. (See related booklet: "Covid-19: A Planning Guide for Labs")
Modular labs design:
Selecting the right module depth and width will be able to help address social distancing. While the 10’ to 12’ module was a basis of design in the past, the preferred module moving forward will be a minimum of 11’, providing the flexibility required to adapt to changing workflows while providing adequate staff separation.
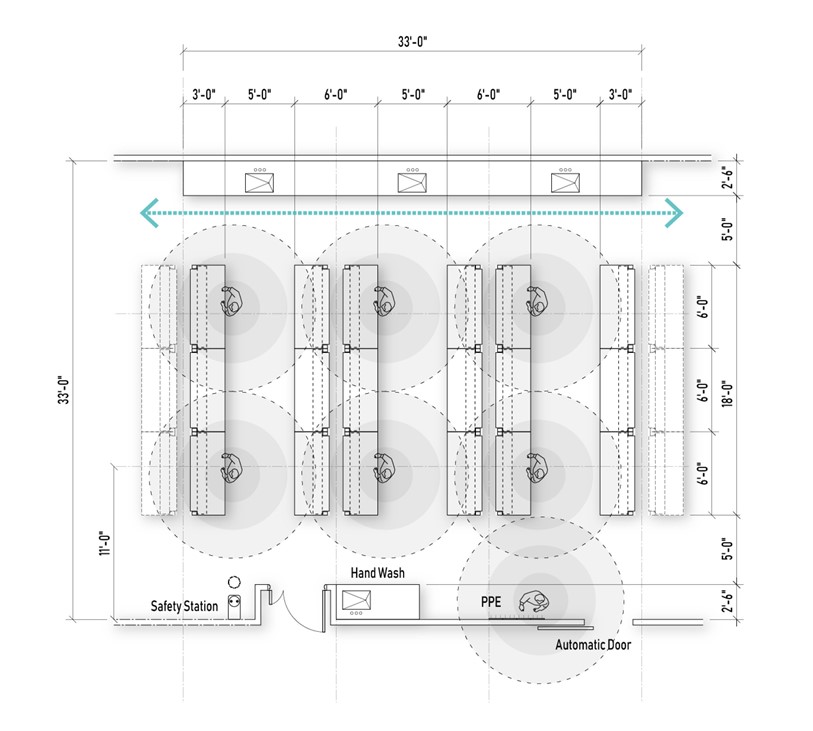
Flexible casework solutions:
Flexible furniture systems will allow the addition or deletion of casework as needs arise to provide isolation by cutting off internal circulation paths, not required by the building code, or removing casework to allow for directional movement between benches.
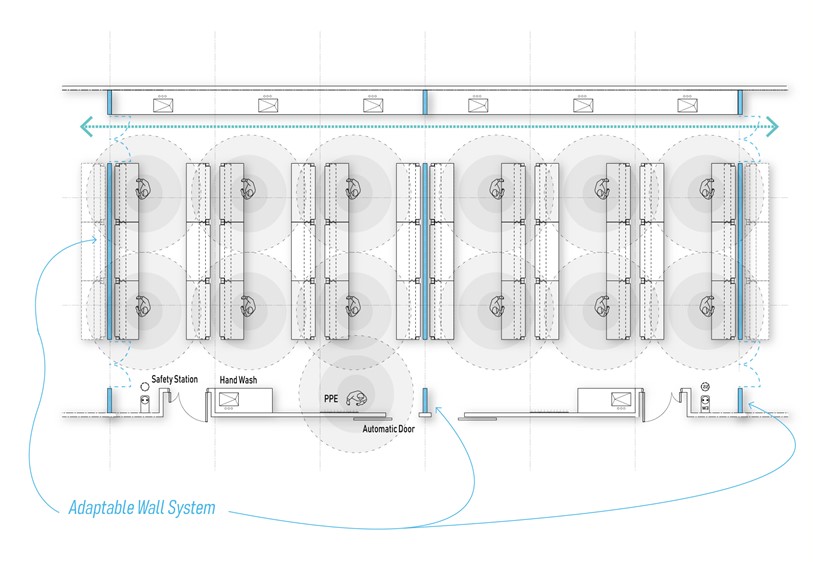
Modular walls:
Laboratory modular wall system allow expansion and contraction of labs based on density requirements. The flexible lab wall system could be implemented in every other module. In times of social distancing, the wall panels could be installed to isolate labs, maintaining interconnection between the now smaller labs by way of ghost corridors. In addition to reducing lab density, a one-way circulation system could be implemented. Once allowed to move back to a pre-Pandemic state, wall panels could be removed, opening the lab back up.
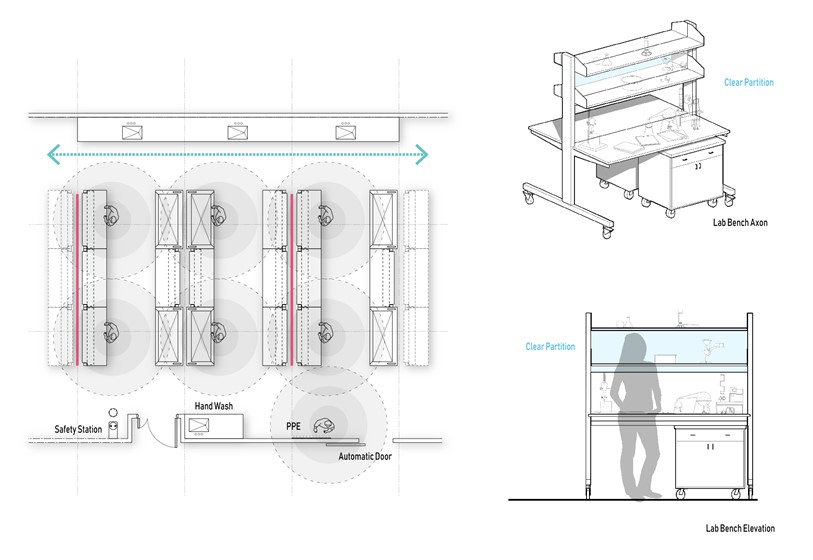
Barriers between staff:
Plexiglass barriers between staff provide separation and allow for visibility and can be mounted perpendicular to the bench, creating 6’- long carols along the bench. Another option is to provide clear plexiglass dividers between benches that would be mounted 24” above the work surface to the bottom of the upper shelf. This acts similarly to a sneeze guard between benches. One caution is to be certain that stagnant pockets of air don't result by adding partitions into the lab space.
Shared equipment zones:
Shared lab equipment is very commonplace, and there is a strong potential for many touch points that can harbor viruses. Strategies to minimize the potential contamination in this area include:
- Determine if there is a way to de-centralize equipment, spreading it out to allow for social distancing. If not, evaluate all interactions and touch points that occur in that zone. Using the hierarchy of controls, determine the appropriate control to minimize exposure. This may be as simple as implementing additional PPE, to creating Standard Operating Procedures for cleaning and sanitizing touch points prior to and after entering shared zones.
- Reorganize the zone to be more efficient based on flow of the process. Possibly reorganize equipment to provide a better workflow, allowing additional space for pieces of equipment that may need extended time for set up, data capture, and clean up and sanitization.
Steps to protect lab personnel from viral spread:
- Stagger lab hours. Limit the number of people in the lab and do all non-lab work at home or in a dedicated space.
Situational awareness. Practice social distancing and respect personnel space. (minimum of 6’, as recommended by the CDC - Clean and disinfect. Set up SOPs to clean and disinfect equipment or areas with heavy interactions, using EPA-approved disinfectants.
- Prioritize hand washing. Wash hands with soap and water for a minimum of 20 seconds before and after using gloves. If sinks are not available, position hand sanitizers close to areas of heavy interactions.
- Wear personal protection equipment. Masks and gloves are known to help mitigate the spread of virus.
- Stay home when sick. Anyone who feels sick should stay home so as not to spread illness. If symptoms are similar to those of COVID-19, contact a doctor and self-quarantine.
- Practice social distancing outside the lab.
